If you are caring for someone with dementia, you already know how much love, patience, and energy it takes to get through each day. When sleep becomes disrupted for them or for you, even small challenges can feel overwhelming. Helping loved ones with dementia sleep better is not always simple, but it is possible with the right mix of consistency, comfort, and gentle guidance.
Sleep changes are common in Alzheimer’s disease and other forms of dementia. Restlessness at night, daytime drowsiness, and episodes of confusion after sunset can leave both the person with dementia and the caregiver exhausted. Understanding why these changes happen is the first step toward calmer evenings. From creating a safe, soothing space to easing nighttime anxiety, small adjustments made consistently can make a meaningful difference in how well both of you rest.
Why Dementia Affects Sleep and Nighttime Behavior

Many people living with Alzheimer’s disease and other dementias experience changes in their internal body clock. The brain areas that help regulate circadian rhythm can be affected, which makes it harder to feel sleepy at night and alert during the day. This shift often shows up as frequent awakenings, daytime napping, or mixed up sleep patterns that leave everyone tired. The National Institute on Aging notes that these changes are common and can vary from person to person.
As evening approaches, some individuals become more confused or agitated. This is often called sundowning. Light levels are lower, routine cues may fade, and fatigue builds. These factors together can increase pacing, calling out, or night wandering. Gentle steps that reduce sundowning at night, such as steady routines and softer lighting, can ease this pattern over time.
Medical and comfort factors also play a role. Pain, reflux, arthritis, urinary urgency, constipation, itching, and untreated sleep apnea can all disturb sleep. Medication timing matters too, including stimulants taken too late in the day or sedating drugs that wear off overnight. A clinician can review medicines and screen for sleep disorders when problems persist. If sleep apnea is suspected, the Mayo Clinic offers a clear overview of symptoms and evaluation.
- Environment: Too much noise, glare, or clutter can trigger restlessness after dark and make it harder to settle.
- Activity balance: Too little movement during the day and long late naps can delay nighttime sleep. Gentle daytime activity helps.
- Light exposure: Bright morning light helps anchor circadian rhythm, while dim evening light supports winding down.
Understanding these contributors makes it easier to plan a dementia bedtime routine that is calm and predictable. Simple changes applied consistently often lower stress and support safer, more restful nights.
Chronic pain is a leading cause of sleep disruptions in old age. Learn how to help your loved one with dementia sleep better despite the pain.
Creating a Dementia Friendly Bedtime Routine

A calm, predictable bedtime routine can make it easier for someone with dementia to relax and drift off to sleep. The goal is to create a familiar sequence of events that signals it is time to rest. This routine should be consistent each night, but flexible enough to adjust for the person’s mood, comfort, and needs.
1. Keep daily schedules steady
Waking, eating, and going to bed at the same times each day helps anchor the body’s internal clock. Even on weekends, sticking to a regular pattern can reduce confusion and improve sleep quality. Aim for mealtimes and medications to be taken on a predictable schedule as well.
2. Encourage light and movement during the day
Exposure to natural morning light helps regulate circadian rhythm, while gentle physical activity such as walking or stretching can promote deeper nighttime rest. If naps are needed, keep them short and earlier in the day. Long late afternoon naps can push bedtime later and may increase nighttime wakefulness.
3. Create a gentle wind down period
Begin winding down about an hour before bed. This might include soft music, reading aloud from a favorite book, hand massage with a familiar lotion, or offering a warm non caffeinated beverage. Avoid television programs with loud noises or intense storylines, and limit screen time that can be overstimulating.
4. Use lighting to set the mood
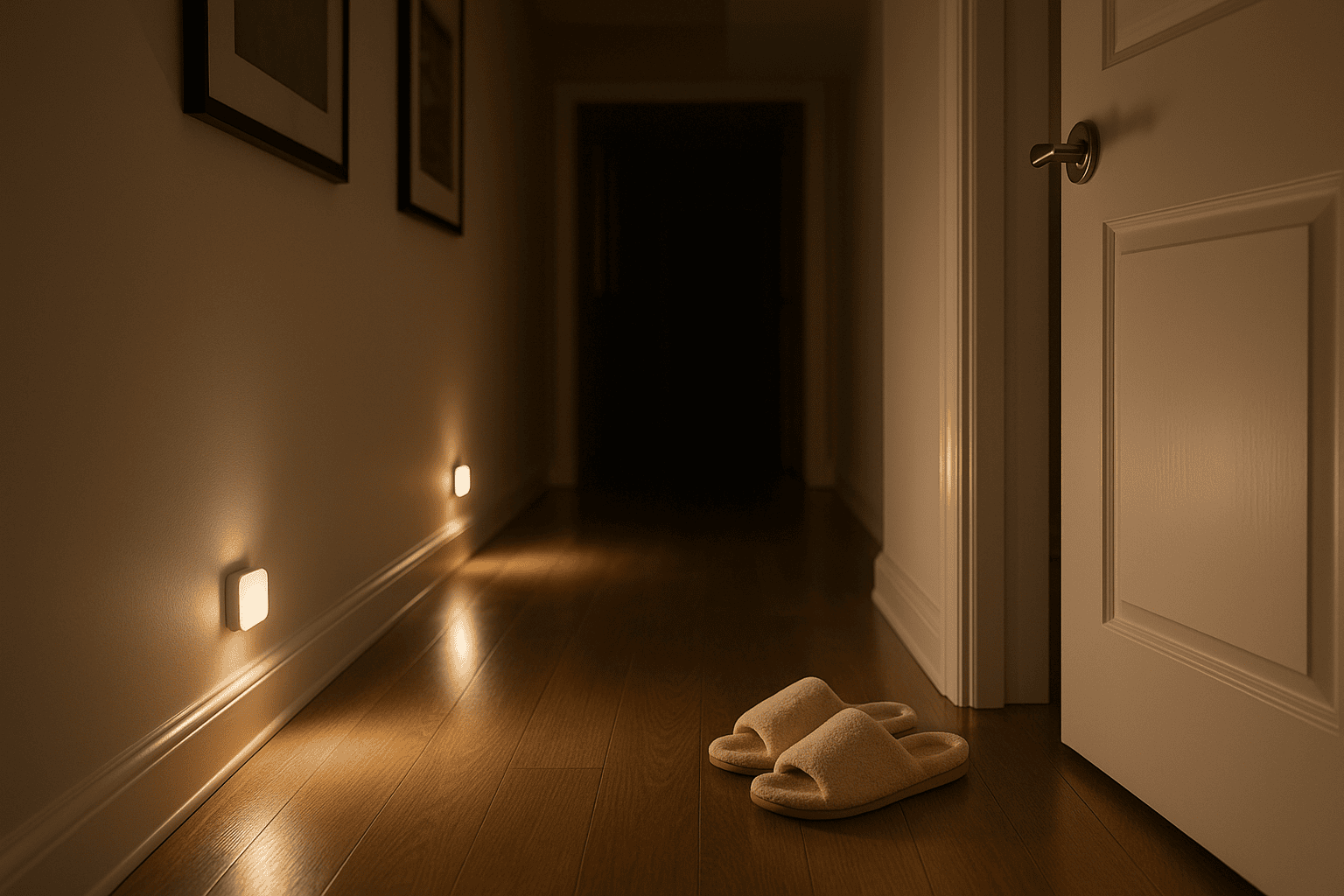
As the evening progresses, switch to softer, warmer lighting. Close window coverings to reduce glare and confusing reflections. Motion sensor nightlights in hallways and bathrooms can guide safe movement if the person wakes during the night and can reduce the risk of falls.
5. Add comfort and familiarity
A favorite blanket, a well loved pillow, or a comforting object can help ease anxiety. Weighted blankets can create a sense of security and calm for some individuals. Keep the bedroom a little cooler and choose breathable bedding to reduce overheating, which can trigger awakenings.
When these steps are practiced regularly, they form a dementia bedtime routine that can reduce sundowning, limit night wandering, and help both the caregiver and the person with dementia enjoy more peaceful nights.
Helping your loved ones maintain good sleep hygiene isn’t easy. We break down everything you should know in our extensive guide on sleep hygiene for seniors.
Safety and Comfort Measures for Night Wandering
Night wandering is common in dementia and can be stressful for caregivers. While it cannot always be prevented, there are practical steps to make the home safer and more comfortable when it happens. The goal is to protect the person from injury and gently guide them back to bed without adding to confusion or fear.
1. Keep pathways clear and well lit
Remove clutter, electrical cords, and small furniture from walking routes. Use nightlights or motion activated lights in hallways, bathrooms, and bedrooms so the person can see clearly if they get up during the night. Place a clear sign on the bathroom door if wayfinding is difficult.
2. Make the bedroom a secure and calming space
Place familiar objects within view to provide orientation, such as framed photos or a favorite chair. Lower the bed to reduce fall risk and choose sturdy furniture that will not tip if leaned on for support. Keep a water carafe, tissues, and glasses within easy reach to reduce unnecessary trips.
3. Install safety devices as needed
Consider door alarms or motion detectors to alert you when the person is up. For exterior doors, locks placed higher or lower than eye level may reduce the risk of wandering outside. Always balance safety with the person’s dignity and freedom of movement. The Alzheimer’s Association offers practical guidance on wandering and home safety in its caregiver resources at alz.org.
4. Address possible triggers
Discomfort, thirst, the need to use the bathroom, or feeling too hot or cold can lead to waking and wandering. Providing a glass of water, adjusting the room temperature, or encouraging a bathroom visit before bed can help minimize these interruptions. Review evening beverages to limit excess fluids close to bedtime if nocturia is a problem.
5. Respond with reassurance
If wandering occurs, guide the person back to bed calmly. Avoid arguing or correcting them, as this can increase agitation. Gentle verbal cues, a warm touch, and a familiar object can help ease them back into sleep. If they seem hungry, a small bland snack may be soothing.
Taking these precautions supports safety during the night and creates an environment where both the person with dementia and the caregiver can rest with greater peace of mind.
A safe and familiar environment is vital for seniors with dementia. Learn how to create a safe and comfortable sleep space for your loved ones here.
Supporting Caregiver Rest and Well Being

Caring for someone with dementia can be deeply rewarding, but it often comes with long stretches of broken sleep and physical exhaustion. Over time, this can affect mood, concentration, and overall health. Prioritizing your own rest is not selfish. It is essential for sustaining the energy and patience needed to provide good care.
1. Accept help when it is offered
Friends, family, or neighbors may be willing to spend a few hours with your loved one so you can rest. If possible, schedule these breaks regularly to give yourself time to catch up on sleep or simply recharge. Keep a short list of tasks that others can do so it is easier to accept help in the moment.
2. Explore respite care options
Adult day programs, in home aides, or short term respite services can give you extended periods of rest without compromising your loved one’s safety or comfort. Even one or two days a month can make a visible difference in energy levels and patience.
3. Maintain your own healthy sleep habits
When your loved one is sleeping, resist the urge to fill that time with chores. Keep your own sleep environment dark, quiet, and comfortable, and aim for a consistent bedtime. Simple relaxation techniques such as deep breathing or gentle stretching can help you fall asleep more easily. If worry is keeping you up, try writing a short to do list for the next day to clear your mind.
4. Watch for signs of burnout
Persistent fatigue, irritability, or feelings of hopelessness may be signs you need more rest or support. Talk with your doctor or a counselor if these feelings become frequent, and consider joining a caregiver support group for shared strategies and encouragement. Many caregivers find that peer support improves coping and sleep over time.
By protecting your own well being, you not only safeguard your health but also strengthen your ability to provide consistent, compassionate care.
When to Seek Medical Advice

Even with the best routines and a supportive environment, some sleep problems in dementia require professional guidance. Knowing when to involve a healthcare provider can prevent small issues from becoming larger health concerns.
1. Persistent or worsening sleep disruption
If your loved one is awake for much of the night despite consistent routines, it may be time to discuss the problem with a clinician. Sleep studies can help identify treatable issues such as sleep apnea or restless legs syndrome. A thorough medication review can also uncover timing problems or side effects that interfere with sleep.
2. Sudden changes in behavior or alertness
A rapid increase in confusion, agitation, or daytime drowsiness can signal an infection, medication reaction, or another underlying condition. These changes should be evaluated promptly to prevent complications.
3. Frequent falls or injuries at night
Falls can lead to serious complications, especially in older adults. If your loved one is falling or at high risk of falling during the night, seek advice on mobility aids, safety equipment, or medication adjustments. Physical therapy may also help improve strength and balance.
4. Concerns about medications
Some prescriptions may interfere with sleep, either by causing drowsiness at the wrong time or by contributing to nighttime restlessness. A clinician can review the medication list to adjust timing or dosages and consider safer alternatives when appropriate.
Open communication with healthcare providers ensures that sleep concerns are addressed in a way that supports both safety and comfort. In many cases, targeted treatment of an underlying issue can greatly improve nighttime rest for someone with dementia.
Preparing for a visit to the doctor can be confusing, even for seniors without dementia. Help your loved one prepare by reading through our extensive guide on when older adults should see a doctor for sleep problems.
Closing Encouragement

Supporting a loved one with dementia through difficult nights is an act of deep patience and care. Sleep challenges can be frustrating, but progress often comes in small, steady steps. By understanding the reasons behind disrupted sleep, creating a predictable bedtime routine, and making the environment safe and calming, you give your loved one the best chance for peaceful rest.
These changes also protect your own well being as a caregiver. Rest allows you to meet each day with more energy, clearer thinking, and a steadier heart. While not every night will be easy, the combination of consistency, comfort, and kindness can make a meaningful difference for both of you.
Looking for other ways to help your loved one with dementia sleep better? Read through our full library of resources here.